Lumbar herniated disc is one of the most common causes of lower back pain and leg pain (sciatica); 80% of people experience lower back pain at one point in their lives, and this is mostly caused by lumbar hernia. With aging or when movements forcing body are executed, discs between vertebrae forming backbone may slide, and as a result, jelly-like substance inside vertebrae leaks out from ruptured part of the disc, causing lumbar hernia. This may cause back or leg pain, numbness or tingling. Therapeutic options may help recovery including resting, painkillers, spinal cord injections and physical therapy. If the problem persists, or loss of bladder or bowel function occurs, operation might be necessary.
Table of Contents
What is lumbar herniated disc?
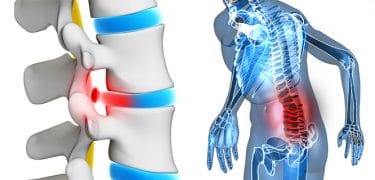
Lower back spine of our body consists of 5 lumbar vertebrae. There is a cartilage called disc between each 2 lumbar vertebrae. With aging or wearing, the discs lose their soft fluids, and become flatter and harder. Known as disc degeneration (damage), this process may start at younger ages.
A jelly-like tissue is present inside the disc. When the back bone is pressured the durable outer ring of the disc gets ruptured. The jelly leaks out of the rupture site, and irritates the spinal cord canal and nerve roots. This is called lumbar hernia.
Causes of lumbar disc herniation
The inflammation of spinal nerves and the pressure of the hernia on the nerve cause lumbar hernia pain. Sciatica is usually a lumbar hernia-related symptom. Pressure on one or more nerves supporting the sciatica nerve may cause pain, burning sensation, tingling and numbness from hip to leg, and sometimes to foot. Sneezing, coughing and bending over usually increases the pain. Usually, one side (left or right) is affected.
Symptoms of lumbar herniated disc
- The mild pain on the back and hip gradually increases
- Increasing pain causes generalized numbness and loss of strength over time
- The pain may hurt the patient very much, and makes their daily life difficult
- The pain decreases within 6 weeks in majority of the cases
- In some patients the pain may be chronic and/or enfeebling
- If the herniated disc is pressing a nerve, a severe pain over this nerve track may be seen. This is also called sciatica and it is the most common symptom in lumbar hernia
Though rare, the symptoms of lumbar hernia may include loss of bowel or bladder control. If this occurs, you should seek immediate medical help.
Lumbar disc herniation pain
Leg pain
It is worse than the back pain. If the pain is spread over the long sciatic nerve track behind the leg, it is termed sciatica or radiculopathy.
Neuralgia
One of the most striking symptoms is neuralgia seen on legs and causing burning, searing, electrocuting or stinging sensation.
Various locations of symptoms
Based on the location and grade of the hernia, the symptoms may be observed in lower back, calf, the front or back of the leg, hip, foot and/or toes, and typically affect one side of the body.
Neurological symptoms
Numbness, needle stick sensation, weakness and/or pins and needles may be observed on leg, foot and/or toes.
Foot drop
The neurological symptoms caused by lumbar hernia may include difficulty in lifting up the leg when walking or standing on toes. This is also called “foot drop”.
Lower back pain
Lower back pain may be seen, however it is not a must. Lower back pain can be defined as constant or throbbing, and you may have difficulty with bending over. If the herniated disc is causing lower back muscle spasm, one or two days of bed-rest may be necessary to alleviate the pain.
Applying ice or heat may also alleviate the pain. You should use a chair with back support when sitting, and support the lower back by lying on your back with a pillow under your knees when sleeping.
Pain getting worse with movement
Standing up or sitting down for a long period of time, or even walking short distances may trigger your lower back pain. Laughing, sneezing or another sudden movement may increase pain.
Pain getting worse with bending over
In many individuals, positions hanging down from a chair, bending over or bending double greatly increase the leg pain.
Sudden pain
Herniated disc pain usually develops very fast, and sometimes, there may not be an apparent movement or incident triggering the pain.
Loss of bladder or bowel control
This symptom is very rare, and caused by the pressured spinal nerve roots. It is a very serious problem, requires immediate medical intervention, and the individuals suffering from this should seek immediate medical help.
Lumbar hernia symptoms usually become more severe when the hernia is affecting a large area. If the disc herniation does not affect a nerve, the pain may be mild and is limited to lower back area. In some conditions, lower back or leg pain continues for a few days and then resolves. This may suggest the onset of lumbar hernia.
Diagnosis of herniated disc
To determine whether you have lumbar hernia, your physician would first want to learn your medical history. He/she performs a physical examination to help with the diagnosis, and if he/she deems necessary, he/she may request a magnetic resonance imaging (MRI) screening for confirmation.
- Medical history and physical examination: After talking about your symptoms and medical history, your physician examines your spine. During physical examination, he/she may perform the following tests to accurately diagnose the cause of your lower back pain.
- Neurological examination: Physical examination should include a neurological examination to determine weakness or sensorial loss. To test the muscle weakness, your physician requests you to walk on your heel or toes. Your hip, ankle and toes should be examined. Your physician touches your leg or foot to determine whether there is a sensorial loss. Checking to see if there is loss of reflex on your knee and ankle is important.
- Straight leg raise (SLR) test: This examination helps a lot in the accurate diagnosis of lumbar hernia in patients below the age of 35. In this test, you lay down on your back, and your physician lifts your aching leg up with your knee in straight position. If you feel pain on your leg and below your knee, it means you have lumbar hernia.
- Imaging Tests: To help with the confirmation of lumbar hernia diagnosis, your physician may request a magnetic resonance imaging (MRI) screening. This screening allows to take clear images of soft tissues such as discs.
Lumbar herniated disc treatment
Today, it is possible to treat lumbar hernia using different method; there are many options from physical therapy to medical therapies, from surgery to micro-surgery. The choice of treatment is based on the condition and severity of the disease. In many cases, lumbar hernia spontaneously improves slowly within days or weeks. Typically, while many of the patients do not develop symptoms, some patients experience pain during recovery period.
Non-surgical (non-operative) therapy
Preventive care should be considered as the first choice of treatment unless there is muscle weakness, walking difficulty, or loss of bladder or bowel control (cauda equina syndrome). The main objective of non-surgical therapy is to reduce pain.
Non-surgical measures in lumbar hernia include
- Resting: Usually, 1 or 2 days of bed-rest alleviates severe back pain. Do not stand up for long periods of time. Rest throughout the day at regular intervals, however, do not sit down for long periods of time. Move slowly and cautiously. Avoid movements which may cause more pain especially such as lifting heavy things or bending over by changing your daily activities.
- Painkillers: Medications such as ibuprofen or naproxen may reduce your pain.
- Physical therapy: If your doctor recommends physical therapy, he/she should communicate the physical therapy specialist about the therapy he/she sees fit to Physical therapy consists of a combination of treatments which are necessary to reduce pain and increase flexibility. Some examples include ice and heat therapy, gentle massage, stretching and pelvic floor, however, your physical therapist works with you to develop the best treatment plan for pain and other symptoms. And good news: Majority of the patients experience an improvement in symptoms without surgery within 4-6 weeks.
- Epidural steroid injection: In this procedure, steroid is injected into your back to reduce local inflammation. Among the measures mentioned above, only epidural injections have been demonstrated to be effective in reducing symptoms. In 42-56% of the patients who received non-surgical therapy for 6 weeks and did not benefit from the treatment, there are strong evidence suggesting epidural injections might be successful.
Herniated disc surgery
Only a small proportion of lumbar hernia patients requires operation. Spinal surgery is only recommended to patients to whom non-surgical therapy was administered previously but failed.
Microdiscectomy
The most common surgical procedure for herniate lumbar disc is lumbar microdiscectomy. Microdiscectomy involves the removal of the herniated part of the disc and all pieces pressing the spinal nerve. The pressure is reduced by providing a larger space for the nerve root, and recovery may start in the nerve root.
Microdiscectomy procedure is usually very successful in alleviating the leg pain caused by the herniated disc (sciatica). While it takes a few weeks or months for the nerve root to have complete recovery, the patients are usually relieved of leg pain fast and experience very little complications after the surgery.
Rehabilitation
Most patients do not require physical therapy after the surgery. After your surgeon evaluate you and confirm that your surgical incision is healed, you can start a rehabilitation exercise program.
As a simple program which you can do at home, stretching exercises for your back and legs and a 30-minute simple walking program will help you heal faster after the operation. If necessary, your surgeon may recommend you a physiotherapist.
Risks of lumbar herniated disc surgery
The only risk of non-surgical therapy is the long period of time taken for symptom improvement. If you choose to undergo operation approximately 6 months later, the outcome may not be as good as if you had chosen to undergo operation before. The risk of surgical complications is extremely low. Possible complications include:
- Infection, Nerve damage
- Dural leak: Laceration of the thin lining of the nerve root canal may result in loss of the fluid rinsing the nerve roots (cerebrospinal fluid). If noticed during the operation, the lining can be repaired. Sometimes, headache is seen after a period of time, however, usually improves over time.
- Hematoma causing nerve compression: This is caused by the blood collected around the nerve roots after the operation.
- Recurrent lumbar hernia: Another part of disc material at the same region may break off, and bring back the leg pain. If preventive care does not provide benefit in this situation, another surgical intervention may be necessary.
Lumbar disc herniation in pregnancy
Already being a painful condition, lumbar hernia may be even more painful during pregnancy. Interestingly, this is common in pregnant women due to the expected weight gain and increasing pressure on the spine. In some cases, the women do not experience the symptoms of lumbar hernia, and may not feel the presence of it during pregnancy. However, a herniated disc may cause severe pain which may worsen with the development and weight gain of the fetus.
Does pregnancy cause lumbar herniated disc?
First of all, pregnancy rarely causes lumbar hernia. Unless the patient has a severe osteoporosis or recently experienced a traumatic injury of lower back, the possibility of lumbar hernia developed due to pregnancy is low. However, women mostly experience a generalized back pain, and pain caused by the changes of the body and around the spine.
What to do for lumbar hernia during pregnancy?
Women who experience moderate-to-severe lumbar hernia pain during their pregnancy, staying positive and controlling the situation with the help of a specialist is important. Mild-to-moderate hernia cases are usually not problematic for the health and safety of the woman and the baby.
However, severe cases may require treatment or intervention to some extent. The patients should also be aware that lower back pain and pelvic pain is common during pregnancy, especially during the third trimester.
To experience a smooth, trouble-free pregnancy, you should stay positive and educate yourself about the herniated discs. If you are experiencing pain, you can benefit from bed-rest and preventive measures such as safe exercises to avoid more injury or pain.
Herniated disc exercises
Home remedies for herniated disc
- Relax: Find a relaxed position to rest. You may sleep on the floor or on a medium-firm mattress by placing small pillows under your head and knees. Or you can sleep on your side by placing a pillow between your knees. Do not stay in the same position for a long period of time.
- Walk: Take 10-to-20-minute short walks on a level surface (without slope, height or stairs) every 2-3 hours. If you experience pain (especially leg pain), stop walking.
- Use painkillers if necessary: These medications are usually more effective if taken before the pain becomes severe.
- Exercise: Be active and do exercises recommended by your physician or physiotherapist to strengthen your back and return to your usual activity level. Stretching exercise may help to strengthen your muscles to protect your back.
- Try to use heat or ice: While there is no strong evidence showing that heat or ice would help, you can try to see if it helps. Sometimes, it might also be useful to switch between heat and cold. For more: >>> Slipped disk





Thank you so much! I now know where my pain is coming from. You’ve been so helpful to me. 😘